How Can We Help?
Section I: Introduction & Rationale: The Value of MYBRAIN Technology for Individuals With Brain Injury
Brain Injury as a Chronic Condition
The World Health Organization (WHO) defines a chronic condition in the following way:
- a condition that is permanent,
- caused by non-reversible pathological alterations,
- which requires special training of the participant for rehabilitation,
- and/or may require a long period of observation, supervision, or care.
Reference: World Health Organization. (2002). Innovative care for chronic conditions: Building blocks for action: Global Report. World Health Organization
Injury to the brain can evolve into a lifelong health condition, termed chronic brain injury (CBI). CBI impairs the brain and other organ systems and may persist or progress over an individual’s life span. CBI must be identified and proactively managed as a lifelong condition to improve health, independent function and participation in society.”
Reference: Brain Injury as a Chronic Condition. (Brain Injury Professional; 2013, Volume 10, Issue 1)
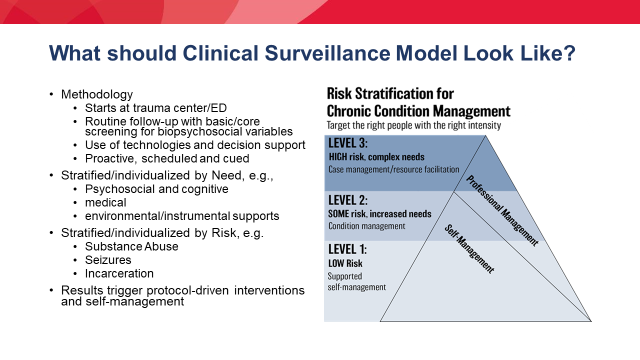
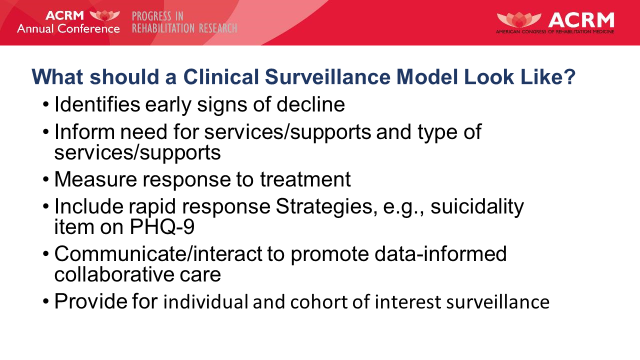
Managing BI as a chronic condition requires:
- clinical surveillance to allow for early detection and intervention for health complications
- surveillance to track participant’s awareness, and readiness for education, intervention and self- management training
- preventive interventions that target high incidence/ high risk complications
- participant engagement & self-management training to improve health and well-being
- access to medical care and rehabilitation services to treat complications and optimize function
Myths about Recovery Exist – Here is what we do know
- recovery trajectories are not the same for all
- recovery is not linear
- recovery is not a simple cause and effect phenomena; multiple factors influence recovery over time including
- premorbid factors such as education, health, age, resourcefulness, adaptability, flexibility
- injury factors such as type and severity of injury
- support/resource factors such as availability of BI specialized resources, access to resources (geography), funding, caregiver engagement, and more.
- life stressors unrelated to the brain injury
- relationship of impaired functions and spared functions to life roles and interests
- recovery does not stop after a few or several months
- progress/success can be facilitated by the right treatments, at the right time, for the right duration, with the right long term supports in place to sustain gains
- research has shown increased issues with aging and acquired brain injury.
Challenges change over time and may include:
- increased frequency of seizures
- decreased trunk control, balance and righting reactions
- increased falls
- dystonia, uncontrollable movement, increased tone
- increased spasticity
- diabetes insipidus
- dysphasia with aspiration
- difficulties maintaining adequate hydration or nutrition
- urinary incontinence
- diminished attention, concentration, memory
- slowed processing, increased disorientation and confusion
- increased need for physical assistance with AM/PM routines and transfers
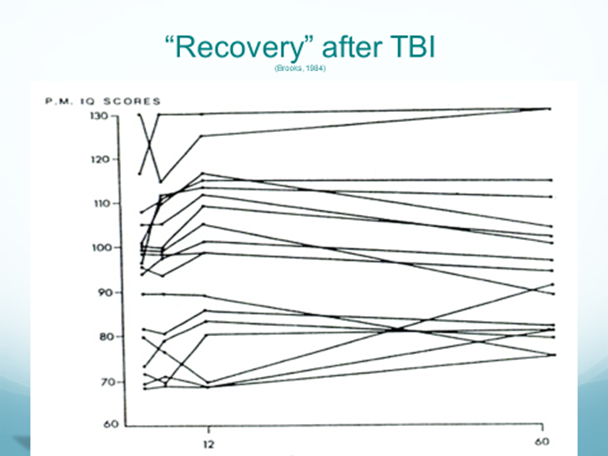
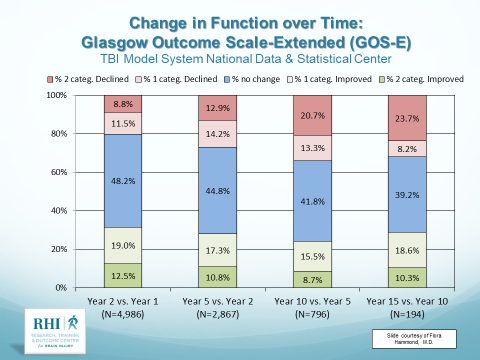
Further, the level of disability that follows from TBI is not static, and change is more common than stability[i]. While 30% of participants will have less disability from one follow-up epoch to another, 30% will become more disabled, and only about 40% will remain stable. Therefore, it was also recommended by the CDC that TBI be proactively managed as a chronic condition.
Comorbidities and co-occurring conditions that affect recovery
The Galveston Brain Injury Conference and the Institute of Medicine, 2 extensive, independent reviews of long term health issues of TBI, results indicated TBI is not an isolated event with a distinct end point, but instead, for some people, marks the beginning of a chronic, often lifelong, medical condition manifested by early mortality, and a host of other comorbidities. Additionally, as noted by the Centers for Disease Control and Prevention (CDC), moderate to severe traumatic brain injury (TBI), as well as multiple mild TBI’s, can result in chronic disability that is associated with both the
primary effects of the injury:
- cognitive or neurobehavioral impairments,
As well as secondary co-morbid conditions:
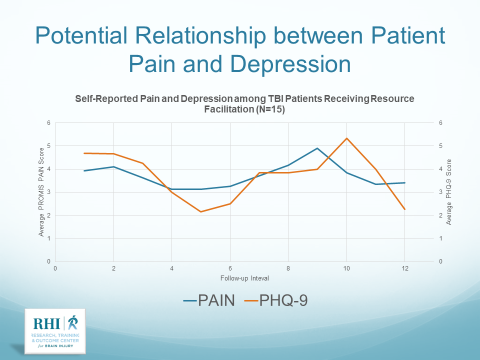
- depression,
- substance abuse
- seizures
- significantly greater health risks-
- including higher rates of diabetes,
- pain,
- insomnia and fatigue,
- hypertension,
- myocardial infarction,
- cerebrovascular disease,
- peripheral vascular disease,
- chronic pulmonary disease,
- and renal disease.
- Substance abuse and psychiatric comorbidities exacerbate the level of disability following TBI.
- People with TBI have been found to be eleven times more likely to die of an accidental opioid overdose.
- TBI is a risk factor for dementia or premature cognitive decline.
- Finally, environmental variables such as lack of access to rehabilitation and brain injury services and supports, lack of family support, and social isolation can result in worsening of disability.
Rationale for MyBRAIN
- As noted, recovery isn’t always recovery, sometimes there is decline
- Awareness is a dynamic, fluid process which impacts engagement throughout recovery
- The individual’s ability to identify needs is often impacted, variable, and at times viewed in the short-term without consideration to long-term implications
- There is a need for prospective, stratified, objective monitoring of an individual’s recovery journey
- Clinical surveillance allows for early detection and intervention for health complications
- Triaged preventive, BI specialized interventions are offered that target high incidence/ high risk complications
- Individualized education is provided as awareness and needs emerge
- Facilitated participant engagement & self-management training improve health and well-being
- Access to medical care and rehabilitation services to treat complications and optimize function
Education efforts geared toward helping individuals with a BI, and their support systems, develop and maintain a self- management plan will help ensure they and their health care partners remain informed and ready to pursue receiving care when needed.